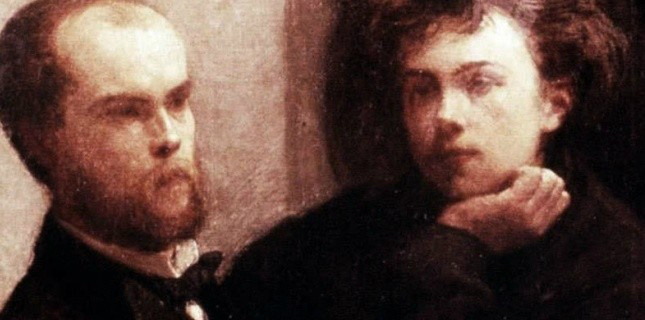
Two Frenchmen in Brussels
- 10. aug, 2014
-
Autant que quiconque
10th of July 1873
Around 2 AM, in a hotel in Brussels, a quarrel arises between two French poets, Paul Verlaine et Arthur Rimbaud. The former, ‘under the influence,’ fires two rounds with his six shot revolver. The latter is hit in the wrist. They go to Sint-Jans hospital where the wound is cared for.
When Arthur wants to go back to France Verlaine draws his gun again, near the Midi railway station. Paul is arrested.
If you want to read some French about the subject of today, click in the title 'Autant que quiconque.'
Over the (h)edge
The Brussels experience
Caring for drug users in general practice: the experience of a general practitioner.
Beyond harm reduction
At the behest of Carl Steylaerts I set out to answer the following questions:
Who am I?
What do I do?
How did I learn?
Why do I do it?
What is the outcome?
Harm reduction
Evidence
Conclusions
Who I am
Dr Peter Van Breusegem
Born 1956 in Asse, Belgium. Promoted KU Leuven 1981. Certified General Practitioner in Brussels for over thirty years.
Most of those years I have been practicing on my own, as a solitary family doctor, alone, were it not for the presence of the people at the front desk.
They deserve to be thanked for their important contribution to the care we provided together to the general public and the substance users alike.
I could not have done what I did, in terms of delivering care for substance users, but for the presence and vigilance of the secretarial staff.
Since a few years we added a second GP position. I am working now in a shared practice with a trusted colleague. This arrangement added much to the comfort of my life.
Surgery
The practice is situated in the center of the busy city of Brussels and serves a varied audience. We see all races, all creeds, all nationalities, all the time. It creates a cosmopolitan climate I cherish.
At the same time it is a needy and impoverished public we see, far from paradise. So we have to deal with all kinds of health problems, which tend to be more common among the poor, and the least is not substance abuse.
The population afflicted by this ongoing scourge is rife with all kinds of medical and other problems, which affect not only the individual but also his or her surroundings; partner, children, family.
Drug abuse is a social disease which is responsible for a devastating wake of suffering and desolation. All kinds of repression have not brought about any sign of relief.
The war on drugs which is being waged for almost a century has had no discernible tempering effect on the epidemic, and causes a lot of collateral damage.
The only way to deal with the problem is care, more and better care, according to modern standards of best quality, highest accessibility and lowest cost.
What I do
So that is what I do:
I am a family physician and I care for families.
In my waiting room the substance user who comes to see me on a regular basis, may be sitting between an old man with hypercholesterolemia and a child with tonsillitis. That is what general practice is all about: anybody might show up and they all need proper and tailored care.
Apart from dealing with nappy problems, work-related stress and irritable bowel disease, I care for a certain number of people on methadone maintenance therapy (MMT.) I have done so ever since 1994, the year the method became semi-legal and ceased to be prosecuted in Belgium.
Taking care of substance users in general practice was a bit of a challenge at the beginning, but turned out to be very rewarding in the end. There is no other category of patients I can think of, who can win so much just by turning to us for care and counsel.
MMT is a cornerstone of the harm reduction approach for some people, but is part of a larger frame, of the inclusive model of primary care medicine, supposed to be open for all and sundry, with a low threshold, and no fuss.
Multifunctional
As a family physician I can address several levels of the problem situation at the same time, which makes my position unique in the care system.
Apart from providing treatment by prescription of regulated medication, I may give my attention to any other health-related problem that comes to the surface.
We all know that substance users in the acute phase often present important health issues, which may have remained unattended, some related to the substances used, others to the way of delivery they choose, like for instance injection, basing or smoking.
We often have to get them to the dentist, take care of respiratory infections, check for hepatitis and so on. We look after their administrative and social status, which can be a bit brain teasing in Brussels, the heart of Belgium.
Quite frequently the user presents psychiatric conditions which require particular attention. Depression, anxiety disorder, bipolarity, psychosis and several personality disorders, to name but a few clinical syndromes, all come to mind.
How did I learn?
Not from school
I hardly ever learned anything useful about the care for substance users during the entire education and training process I went through before I graduated.
Judging by the level of knowledge displayed by the students I see during the practical training hours I coach, they know more about everything than I ever did, with the notable exception of drug use and its management, suggesting the curriculum doesn’t get much better in this respect.
Twenty years ago I was in a kind of crisis situation. I had just taken over a surgery in the center of Brussels, and was confronted with a rather large population of substance abusers. Luckily I realized immediately how ill prepared I was, and I looked around to learn more about the issue.
I had to learn how to manage this kind of problem, and after some field research, the best choice proved to be to adhere to a monthly meeting group of primary care professionals, most but not all of them physicians.
We call it ‘Intervision.’ We sit around a table and discuss cases. I do that for twenty years now and it has helped me a great deal, to get better in doing what I do. Every month we meet and share our experience with each other. So that is how I learned the tricks of the trade.
Supervision
The quality of the experience is greatly enhanced by the presence of two supervisors during the intervision meetings. At this time, one of them is a doctor, the other a psychologist. This is of great use to help us understand better what we are doing.
We all know and trust each other. We can get advice on difficult cases, or find support to cope with personal issues. We can compare with our peers how we are functioning. We get feedback and we can express our inner feelings if and when needed.
The feeling of mutual trust has proven to be quintessential in the benefit we got from our monthly meetings. It has been a constant and reliable source of knowledge and constitutes a body of experience I would not want to miss.
We had all kinds of discussions and those helped me make up my mind about what we do and what we should be doing in our clinical work with users.
The very basis of our clinical success is the establishment of the therapeutic relationship, which requires an open mind and built on mutual trust.
Why I do it
Old enough to remember the eighties
We had no MMT then. There was a very strong feeling, in society as in medical circles, against dealing with illicit drug use, which reflected badly on the users. We were supposed to make them feel unwanted.
As a starting GP I was very sad to discover that we could do so little to help those drug users who came to our attention, many of whom presented so many challenging medical and psychosocial problems.
We had not much to offer except good advice, none of which was new to them, and the ill-advised prescription of all other kinds of medication, mostly benzodiazepines, which was a shame because it was bound to become another addiction. So, instead of curing them of one addiction we gave them a second one to go with it.
In 1994 MMT became semi-legal in Belgium. The therapeutic value was publicly recognized and I started to get people on methadone. In some cases the results were quite spectacular.
I witnessed an impressive number of patients on MMT get their lives in order and get a life in the first place. I saw them settle down, go to school, get work, start a family etc.
People on heroin tend to be much more in charge of their lives on MMT and be less at risk for all kinds of complications. They get better and they come back to us, because it works.
Low treshold
This was such an uplifting experience, that I felt this method should not be denied to anyone asking for it. We have to react fast and serve efficiently to provide the treatment, the very moment it becomes clear it’s needed.
There is no time to get the opinion of all kinds of services and consultants. The advantage of the GP is, it can be done there and then. The addiction problem is immediately taken care of, by supplying the necessary pharmaceuticals, which opens the door to all other kinds of care in a later stage.
The central idea is that we should assist the patient in a recovery process which gets him or to function as a social human being, and to be in better control of things.
Providing MMT is no more than another tool to achieve more control and promote the feeling of being in charge.
Outcome
Just another one
Addiction is just a chronic disease like diabetes or asthma.
Science provides the necessary means to deal with all kinds of lasting health problems, and enable those afflicted to live a fruitful human life.
At the positive side, I have known of many people who decided after a short or long period to stop MMT because they felt ready for it. Some come just a few times and get rid of it. Others need more time.
A certain number continue their treatment for many years. Most of those are probably just ordinary citizens who never draw any attention.
Not all of those who ever applied get out of trouble. I often wonder where all of those I have seen over twenty years are today.
Quite a few of our patients are deceased, several of them rather young and we regret a few suicides.
Harm
Others are in prison, or in psychiatric care, or being taken care of by their families.
MMT notwithstanding, drug users remain a population still at more than the usual risk for violence, suicide, overdose etc, not to mention aids and hepatitis.
MMT is not a ride in the park, but it is the single most effective treatment procedure in General Practice I know of, in as much as it offers a better quality of life, enhanced self-reliance, development of social integration, empowerment, harm reduction etc.
I cannot think of any other treatment that brings so many benefits in any population.
Primary care in Brussels plays an important role in the provision of this treatment.
It is low cost, low tech, affordable, near you, accessible, with unlimited capacity. The family physician offers a relation of trust growing over the years. He or she is able to look at different sides of the problem, in medical terms, or from the psychological point of view.
Harm reduction
Success depends on the targets you choose.
Abstinence as a target is sure to fail for a great number of patients. They have all tried to stop, maybe successfully, but not for long. Addiction is per definition the inability to abstain.
Harm reduction is based on the common sense idea that we should not wait for abstinence to occur, before we get in action, and do what we already can, to reduce the harmful consequences associated with the substance abuse.
As far as heroin addiction is concerned, MMT is a corner stone of the harm reduction approach. One effect of it is immediate. You will know what you get, instead of taking a product you do not know what is inside. The substance may be cut or adulterated and the price may vary. The user has no means to check the quality and is never sure to have constant access to something he or she needs on a daily basis.
In MMT the regular services of a physician who prescribes and a pharmacist who delivers assure pharmaceutical quality of the provided substance. The product is pure, the price modest, the availability assured. It’s legal and covered by social security.
This means a great deal to our harm reduction perspective, and it is just for starters.
Global approach
As we work in a primary care setting, we can do more than just prescribe methadone.
During the first meetings we draw up an inventory of all problems and we deal with them one by one according to priority as we go on. This means more harm reduction.
We could propose do some blood testing. In as far as the intravenous users are concerned hepatitis B and C will have to checked, as are syphilis and HIV.
Fortunately we see not so many IV drug users in Brussels as compared to many other places and they seem to become less frequent as time goes by.
The negative consequences of the smoking habit may be of much more consequence. The cardiovascular fitness often leaves much to be desired.
We send them to the dentist and look into other possible health problems. At the same time we get an idea of any signs of mental health disorders and treat those if possible.
We see a lot of psychiatric pathology in this group as mentioned before. It is of great importance that people with a habit of substance abuse find the way to mental health care.
It may take lots of paperwork to get their administrative status in order.
Beyond Harm Reduction
Over the years
Some of my patients I still see today go back the full twenty years of my practice.
Addiction for some is a lifelong problem and in some people it can be treated but not cured. A group of MMT patients kept coming over the years, some of the on very low dose now. We continue as long as it seems to be useful.
These are the ones we know best, and probably care most about. They represent one of the possible outcomes of MMT, that there is no outcome except for going on with it.
Typically, as we get along with MMT, we often see the user get more and more stable, settle down and find some sort of equilibrium.
The items on the to do list may take months to get cleared, which allows for a feeling of mutual trust to develop into a therapeutic relationship.
It is like a cleaning process, you get off the other layers of problems and then you get to the core. With the harm reduction aspect out of the way, we start to know each other better.
We often hear appalling stories of how those people got abused, hurt or damaged in the past. It is very important not to miss the opportunity, and to react adequately, when such issues arise, because this creates a hope of healing.
Rather frequently, a need for psychotherapy will occur. Referral to a therapist happens best at such a time the person feels ready for it.
With Carl Rogers we share an optimistic belief that every human soul if nurtured carefully has a potential of development. By taking away all crusts of misunderstanding and unnecessary defense mechanisms we may hope to free the mind enough so the person can unfold his personality.
We believe that the care system should be emancipatory in nature.
The physician should not only transfer his authority but his knowledge as well, whilst providing the necessary means for people to take control of their lives again.
We often have to take into account as well the needs of the surroundings: parents, partner, children, friends. They may all have their part of healing to do.
Literature
Evidence Based Medicine
There is a wealth of scientific evidence available in medical literature, not only about methadone maintenance treatment as such, but more specifically about its feasibility and efficacy in General Practice as well.
Here are some links.
This is just a handful of articles available on the subject. It is not meant to be exhaustive nor conclusive, but just illustrative
MMT as such
A good place to start is a concise overview article published in 2002 and available on the website of the American Centers of Disease Control (CDC) as a pdf document (no author.) It comes with a lot of links of references suggesting further reading.
http://www.cdc.gov/idu/facts/methadonefin.pdf
It is interesting to see how every country has integrated MMT in its national policy. Health Canada (www.hc-sc.gc.ca) offers a good overview and standard of good practice in that great country. The benefits of MMT are well documented.
http://www.hc-sc.gc.ca/hc-ps/pubs/adp-apd/methadone/index-eng.php#a2.2
Some myths about MMT are addressed in the following link, which turns to the general public. The discussion following the article is instructive about the feelings of the stakeholders;
https://www.drugfree.org/join-together/addiction/commentary-countering-the-myths-about-methadone
The next article asks the question: “General practice or drug clinic for methadone maintenance?” and promises a controlled comparison of treatment outcomes. According to the abstract, the findings “suggest that with similar patient groups this model of care in general practice can produce results at least as good as those of a drug clinic.”
Primary care
MMT in general practice
Here are a few more links
“Methadone maintenance in general practice: patients, workload, and outcomes” is an article in the British Journal of Medicine which looks specifically at the requirements and challenges of MMT in the general practice setting. Conclusions: “Providing methadone maintenance in general practice is feasible. Although costs are considerable, the reduction in drug use, especially of intravenous opiates, is encouraging. Attending clinics also allows this population, in which morbidity is considerable, to receive other health care.”
http://www.bmj.com/content/309/6955/641
“Methadone treatment practices and outcome for opiate addicts treated in drug clinics and in general practice: results from the National Treatment Outcome Research Study,” is the self-explanatory title of the next article. Results “demonstrate the feasibility of treating opiate addicts using methadone in primary health care settings, and show that treatment outcomes for such patients can be as satisfactory as for patients in specialist drug clinics.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1313314/
“Can methadone maintenance for heroin-dependent patients retained in general practice reduce criminal conviction rates and time spent in prison?” Such is the question asked by the next article. “The results support the hypothesis that patients retained in methadone treatment in general practice have a significantly lower rate of criminal convictions and spend significantly less time in prison than before initiation of treatment.”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1313612/
“Methadone treatment for opiate dependent patients in general practice and specialist clinic settings: Outcomes at 2-year follow-up,” is a study from England. Results “show substantial reductions in a range of problems behaviours, among unselected samples of opiate dependent patients treated in GP and in clinic settings, which are sustained to 1-year and 2-year follow-up.”
http://www.journalofsubstanceabusetreatment.com/article/S0740-5472(03)00040-0/abstract
“A decade of caring for drug users entirely within general practice” comes from Bedford, England. “Long-term care of drug users entirely within general practice is feasible. Among those prescribed methadone ampoules, a higher than average proportion had stable lifestyles and had a stable job.”
Finally
In dealing with MMT in a primary care setting I have to give credit for two great privileges I have enjoyed over those years.
One is to have participated in the monthly meetings of our peer intervision group with supervision of two experts from LAMA as we have explained.
The other is to have been of service and hopefully of some use, to a number of people I have seen, because they came to see me with some kind of drug addiction related problem. Some of them I have followed through their lives from the moment they took the turnabout and decided to stop the heroin abuse, until this day as we go on.
The people we see today are the survivors. Other stories ended badly. There is a lot of dramatic suffering in this field. We share their ups and downs, and we stand by as they fight their demons. So many confided in me about their feelings and fears and put their trust in my hands so to speak.
This is a privileged position of great responsibility I hope and strive to be worthy of. All these people together who came to see me over twenty years taught me what I know today. Apart from the intervision group, this is the other great source of learning I enjoyed.
Recommendations
I would like to see better teaching and education of physicians and all other staff about the management of drug addiction related problems.
I would like to transfer my experience and knowledge to the coming generation, as we have the feeling, at our monthly meeting, that there are not many out there to follow our footsteps.
Treatment of heroin addiction should be swift and effective in order to be able to take care of all other problems.
General practitioners should at least be able to look after those patients who come from the very families they care for.
Primary care should be open to all and be inclusive to all kinds of human behavior, including drug use.
Conclusion
Near to you, easy access, affordable, cheap, fast and efficient. The best way out of heroin addiction. Go to your GP if your habit gets to be a problem.
We may hope that the education and training of GP’s will address the need for more skills and competences in the management of drug users.

Meest recente commentaren